What is hydrocephalus? And how can neuro42 help treat it?
Cerebrospinal fluid, also known as CSF, is a clear and colorless fluid surrounding the brain and spinal cord. It is a critical component of the body’s central nervous system, removing impurities and protecting our delicate brain and spine.
But when it comes to CSF, you can have too much of a good thing. And when that happens, it results in a condition called hydrocephalus. In today’s post, we’re going to explore the topic of hydrocephalus, explaining what it is, why it occurs, how it’s diagnosed and how it’s treated.
What is hydrocephalus?
The word “hydrocephalus” is derived from two Greek words—“hydro,” which means water, and “cephalus,” which means head. According to the Hydrocephalus Association, the condition “affects over 1 million Americans, ranging from infants and older children to young and middle-aged adults, as well as seniors.”
So, just what is hydrocephalus? Like the etymology would imply, it involves water in the brain. Except, in this case, the water is the cerebrospinal fluid we talked about earlier.

Why does hydrocephalus occur?
The answer to how hydrocephalus occurs will vary depending on which of the two main types we’re talking about: congenital or acquired. Congenital hydrocephalus, recognized in utero or early in life by a pediatrician, means that the child is born with the condition. On the contrary, acquired hydrocephalus is the result of something that occurs after birth.
Common causes of congenital hydrocephalus include spina bifida, aqueductal stenosis and brain malformations, while head injuries, brain tumors, brain bleeds and infections of the brain or spinal cord are prone to causing acquired hydrocephalus.
In general, hydrocephalus occurs when there’s an imbalance between the amount of CSF the body produces and how quickly it is absorbed. CSF continually circulates throughout our ventricular system and becomes absorbed into our bloodstream. But when it unnecessarily accumulates, those ventricles will swell and the pressure inside the head increases, causing the patient’s head to enlarge.

How is hydrocephalus diagnosed?
Like many neurological conditions, hydrocephalus is diagnosed through the use of brain imaging techniques, based on age, symptoms and known or suspected abnormalities. In some cases of congenital hydrocephalus, a prenatal sonogram or ultrasound may be able to diagnose the condition before the child is even born.
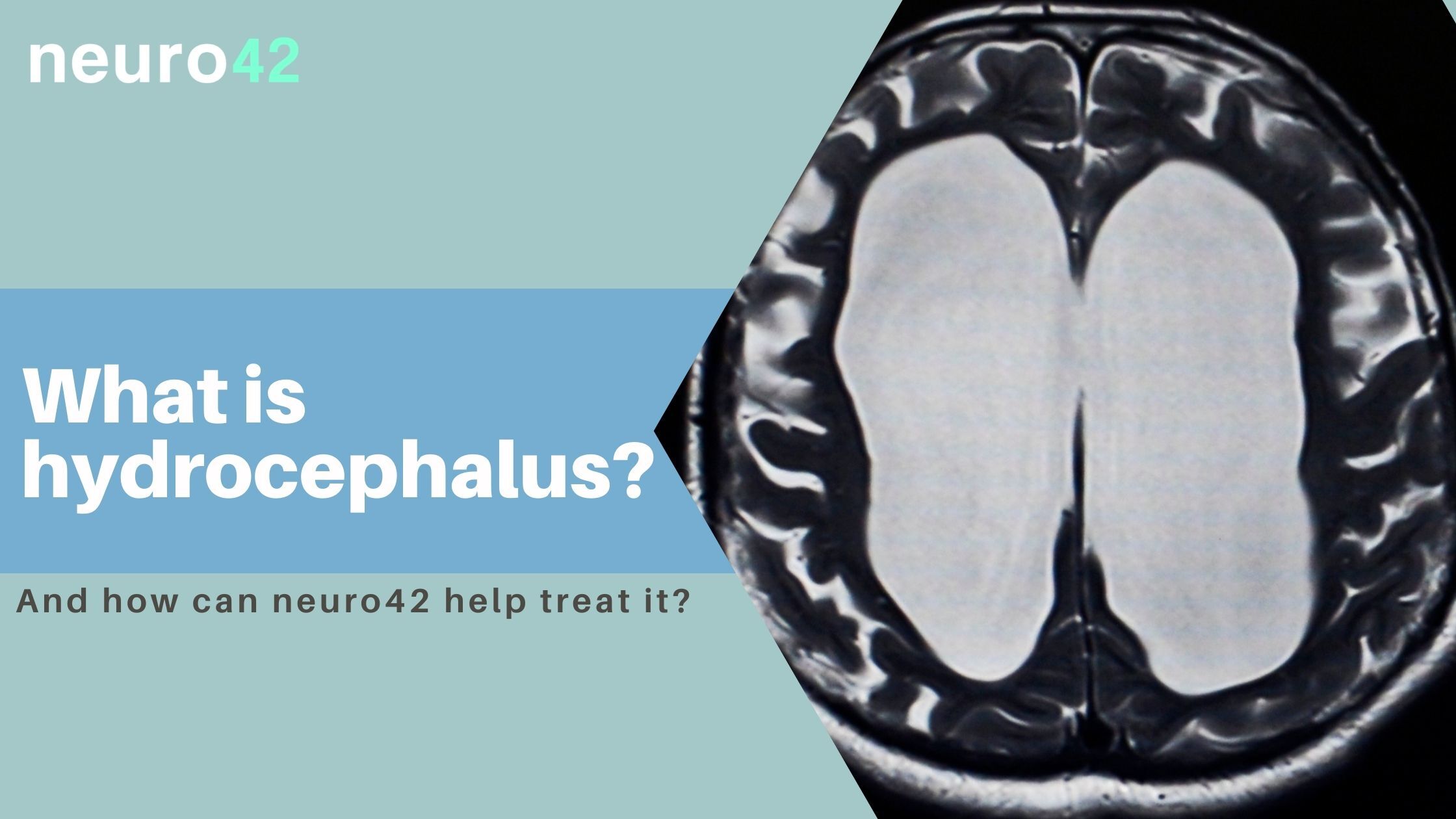
MRI, which is among the first tests used in adult hydrocephalus, can identify if the ventricles have swelled and to analyze CSF flow patterns. CT scans are another form of imaging that doctors use to diagnose the condition.
In addition to imaging modalities, a lumbar puncture (also known as a spinal tap) may be performed to estimate CSF pressure as well as a neurological exam to check muscle strength, vision, mental functioning and other vitals.
How is hydrocephalus treated?
Hydrocephalus is the most common reason for brain surgery in young children. The insertion of a shunt, a drainage system consisting of a tube and valve that helps the CSF flow properly, is frequently used to treat the condition. For patients who do have a shunt surgically inserted, regular monitoring is required for the rest of their lives.
One of the most significant complications in the insertion of a shunt is ensuring it is accurately placed within the brain. Fortunately, surgeons have discovered that using intraoperative imaging can allow them to place the shunt more precisely.
Published in the Journal of Neurosurgery, one scientific study spanning a 10-year period found that, “The odds of highly suboptimal or unacceptable placement were significantly increased by lack of any intraoperative imaging…” Further, the authors concluded that using intraoperative imaging for how and where to locate the shunt “may optimize outcomes by avoiding the majority of unacceptable placements.”

neuro42 aims to provide better outcomes for pediatric hydrocephalus patients
At neuro42, we’re particularly passionate about the treatment of pediatric hydrocephalus because the opportunity for improvement is so ripe. It has been reported that there are some 10,000 pediatric hospital admissions for shunt malfunctions each year, and about half of all shunts in the pediatric population fail within two years.
Knowing what we know about the effect that intraoperative imaging can have on shunt placement, we believe neuro42 can profoundly impact the future of pediatric hydrocephalus. Powered by intelligent procedural planning and predictive analysis, our technology will aid surgeons with intraoperative robotic guidance under live imaging.
Patients shouldn’t have to undergo multiple surgeries simply because a shunt wasn’t placed exactly right—and with neuro42, they may not have to.
